BY PAM MCGRATH
ILLUSTRATION BY ABIGAIL GOH | PHOTOS BY JAY FRAM

For the sick it is important to have the best.
Taking care of sick people is hard. Whether you’re staying home with a kid who has a fever, spending the weekend with a friend and her broken ankle or helping a parent age at home, the task, though done with love and concern, can take a toll.
That simple truth applies to professional caregivers, too. And because caring for someone is hard work, many who choose the field of health care don’t view the profession as a job; rather, they feel it is a vocation, a calling to minister to people in need.
But those on the front line of care and those who provide support services for them are as human as the rest of us. The rewards of seeing seriously ill patients regain their health are heady; the reality of witnessing prolonged suffering and death can cause pain. The challenge for health care institutions such as Barnes-Jewish Hospital is to take care of not only patients, but their caretakers, to make sure the rewards continue to dominate the reality.
Like many hospitals across the country, Barnes-Jewish Hospital offers its patients a staff of excellent nurses. It has earned Magnet designation — the highest level of recognition for hospital nursing — at every four-year evaluation since 2008. And the hospital has come to recognize that its nurses can help the hospital achieve its mission — to take exceptional care
of people — only when they are cared for themselves. To that end, Barnes-Jewish Hospital, among other health care institutions, has developed programs aimed at ensuring its caregivers receive the care and support they need to retain their excellence.
Barnes-Jewish Hospital’s approach is twofold: Its WeCare program offers immediate peer assistance when difficult situations arise; and its Building Resiliency for Compassion Fatigue series of classes helps caregivers acquire the psychological tools they need to cope with daily challenges.
The consequences of compassion fatigue
Compassion fatigue in the field of health care occurs when professionals feel depleted physically, emotionally or spiritually as a result of caring for patients who are in emotional and physical distress. Two factors contribute to compassion fatigue. The first is secondary traumatic stress — also known as second victim trauma — brought on by repeated exposure to trauma experienced by others. Profound examples of incidents that caused secondary traumatic stress for people across our nation were the shocking images of the Sept. 11, 2001, terrorist attacks on the World Trade Center in New York or, more recently, of children fleeing from an active shooter in their schools. More personal experiences, such as witnessing a fatal car accident or violent altercation, may also cause secondary traumatic stress. The emotions these kinds of incidents provoke can remain with us for days, even months, to come.
“These experiences create a kind of holographic image in your head that plays repeatedly,” says Catherine Powers, MSN, RN, a clinical nurse specialist in the Washington University and Barnes-Jewish Heart & Vascular Center and a resiliency-training specialist. “Similarly, caregivers can experience incidents that have a profound impact on their psychological well-being.”
The second contributing factor to compassion fatigue is burnout, the chronic condition by which perceived demands always outweigh perceived resources. For those experiencing burnout, there is never enough staff, equipment, time — a host of “fill in the blank” deficits.
The result of these combined factors is compassion fatigue, which may manifest itself in myriad ways: mental and emotional exhaustion, insomnia, headaches, nausea, difficulty concentrating, rapid heartbeat, isolation from others, depression, anger and irritability, self-doubt.
It may seem impossible to avoid compassion fatigue, especially in a tertiary care setting like Barnes-Jewish Hospital, where staff provide highly specialized care for complex medical issues.
It is not.
WeCare on call
Michele Gatzert, DNP, MSN, RN, clinical nurse manager for an intensive care unit at Barnes-Jewish Hospital, remembers precisely when the concept for a peer-driven support team began to take shape in her mind.
“There was a medication complication that resulted in a patient’s death. There were a number of contributing factors, including a hectic day with multiple interruptions in care,” she says. “The nurse involved was highly trained and experienced. It was devastating for her, but then there was another factor that intensified her response: She was single, so she was going home to an empty house to deal with her feelings alone. There had to be a better way to help caregivers like her handle these emotionally wrought situations.”
Research led Gatzert to Susan Scott, PhD, RN, who established the forYOU peer support team for University of Missouri Health Care. It was the first of its kind when launched in 2009; similar programs now exist at Johns Hopkins Hospital in Baltimore, Beth Israel Deaconess Medical Center in Boston, and a growing list of others.
Building on the insight she gained from Scott’s experience, Gatzert based her doctoral thesis on developing a similar program at Barnes-Jewish Hospital that incorporated a two-tiered approach. Tier 1 promotes basic emotional first aid within the hospital’s local or departmental level. Tier 2 ensures prompt availability and access to professional counseling support and guidance.
“The people who best understand what nurses experience in health care — unexpected patient outcomes, a first patient death, even a threat of harm — are those who work alongside us as our peers,” says Gatzert. “WeCare volunteers enhance coping by providing a ‘safe zone’ in which those dealing with difficult situations can express their thoughts, reactions and feelings.”
Examples of how WeCare volunteers have helped Barnes-Jewish Hospital caregivers and support staff illustrate the highly emotional and sometimes volatile situations that are the reality of patient care: Within 12 hours, a teenager who overdosed on Tylenol went from needing a transplant to becoming an organ donor, and Sarah M., a nurse, helped the grieving mother hold her daughter one last time. Tina G., a soon-to-graduate nursing student, witnessed her first death after performing CPR for the first time on a patient. Aisha J., a member of the housekeeping staff, witnessed the grief of a stillborn baby’s parents, a wrenching reminder that she had recently lost a grandchild. Georgia P., an agency nurse present when a critically ill patient died, endured an aggressive reaction — “You killed our mother!” — from the woman’s daughters. The only reason she returned to work the next day was because of the support she received from her peers afterward.
Gatzert says, “My own experience involved a young girl whose mother had terminal cancer and was close to death. Suddenly the alarms on the monitoring equipment went off, and the girl yelled, ‘What is going on?’ She ran to me, wrapped herself around my legs and said, ‘Don’t let my mommy die.’” Gatzert was traumatized by the experience and ended up in the bathroom, alone, crying. “Almost immediately there was a knock on the door — another patient was being transported to the ICU from the ER. I had to get back to work.”
She adds, “It was 16 years before I told anyone that story. And that’s what used to be the measure of a good nurse — being tough and showing no emotion because that’s how you survived the job. That is the attitude we are changing with our WeCare initiative.”
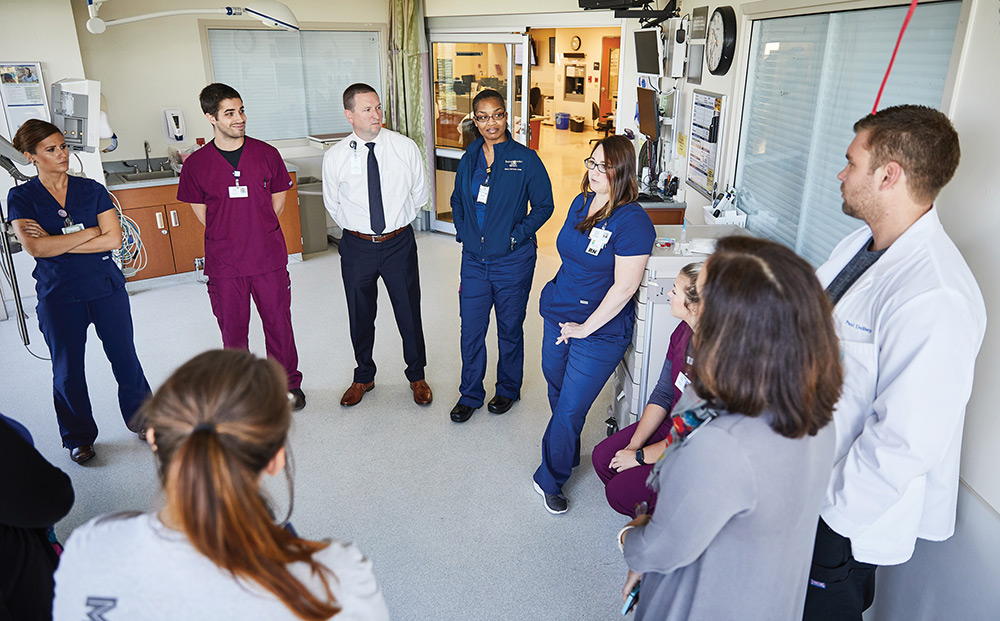
MEMBERS OF THE WECARE TEAM AT BARNES-JEWISH HOSPITAL MEET TO CONSIDER PATIENT NEEDS.
At its inception in 2016, the WeCare team included just Gatzert and two other volunteers. Since then, the team has grown to more than 100 volunteers, from staff nurses and nurse managers, physicians, chaplains and clinical psychologists to representatives from human resources, patient safety, employee assistance and media relations. Volunteers attend workshops that create awareness of the second-victim phenomenon, offer aspects of peer support and teach interventions employees can use to help one another.
“Sometimes I receive calls from individuals asking for help, but often it is a co-worker who tells me someone may be in trouble,” says Gatzert. “That person may not want to talk immediately, and that’s fine. I give them time and then check back to see what kind of help they need.”
For some, that means a referral to professional counseling through the employee assistance program, or time spent with a chaplain, social worker or clinical health psychologist.
WeCare averages 300 to 500 employee encounters each year. An initial analysis of outcomes in 2016 showed that of 169 employees, 26 mentioned leaving their profession and 40 talked about leaving their work environment. A follow-up showed that only nine had left either their profession or work environment.
In January 2018, The Joint Commission, a nonprofit organization that accredits and certifies health care organizations and programs in the U.S., issued a recommendation for hospitals to establish programs supporting health care workers at risk for developing compassion fatigue.
“It’s not that the health care world is full of people who are burned out or in compassion fatigue. It’s called life,” says Gatzert. “Imagine what it might feel like if the emotions you experience seeing a traffic accident become part of your job every day. Sometimes people just need help processing emotions so they can continue to be productive. Through WeCare, we have humans taking care of humans.”
Tools for avoiding compassion fatigue
The hospital’s six-hour class called Building Resiliency for Compassion Fatigue is designed to help caregivers avoid compassion fatigue by heightening awareness of its symptoms and providing skills for combating the stress arising from working in a challenging environment.
“The hospital’s focus on resiliency was in response to a tragic death witnessed by oncology nurses working with patients receiving chemotherapy,” says Powers. “This was traumatic for nurses who were working in an area where deaths normally didn’t occur. Their nurse manager approached Patricia Potter, RN, PhD, then director of research for patient care services, and asked if she could find out what could be done to support employees experiencing that kind of second-victim trauma.”
A research team led by Potter and Teresa Deshields, PhD, formerly the manager of the Counseling Service at Siteman Cancer Center, undertook a study into the prevalence of compassion fatigue and burnout among oncology nurses. Their work led to a consultation with J. Eric Gentry, PhD, a traumatologist and expert in the area of compassion fatigue, who also is the consulting director at the Traumatology Institute. In 2011, Gentry helped develop the hospital’s Building Resiliency for Compassion Fatigue class. To date, more than 1,200 caregivers and support staff from Barnes-Jewish Hospital and facilities throughout BJC HealthCare have attended the class.
“We explain to participants that our goal is to get them back to that person who said, ‘I want to be a nurse, a physician, a patient care tech, a social worker, an emergency room security guard.’ That level of excitement was there when they began their careers,” says Powers. “That is a person’s real self. It’s not the tired, stressed-out person who is depressed or having nightmares because of something they experienced at work.”
Powers emphasizes that it’s not just those working in health care who can be negatively impacted by their work. People in all kinds of professions experience stress, and there is a physical change in the brain when it happens.
“It’s called sympathetic nervous system domination, or the fight or flight response. It changes a person’s cognitive function,” says Powers. “Our class provides those attending with skills that act like antibodies, including stress-reducing techniques that help them relax and bring them back to their normal reasoning.” These antibodies focus on self-regulation, perceptual maturation, social networking, intentionality and self-care outside of the workplace.
“Another significant section of the class encourages participants to share their experiences and the significance these have in their health care journey. Admitting they have been affected by their work as a caregiver is an important step toward feeling better,” says Powers. “We further support that healing by asking people to write their covenant, to define why they are here on earth and how they visualize how they want to live. It’s another way of bringing them back to who they really are.”
Prior to taking the resiliency class, participants are asked to fill out a professional quality-of-life survey that measures burnout and secondary traumatic stress. They are asked to complete the same survey within six months of taking the class. In a sample comparing the surveys of 164 participants before and after the class, the percentage of nurses with burnout risk fell from 24.1 percent to 18.8 percent and for all other disciplines from 19.2 percent to 11.5 percent. Secondary trauma risk for nurses dropped from 40.2 percent to 32.1 percent and for all other disciplines from 30.8 percent to 23.1 percent.
“Resiliency training can be helpful for anyone, from nursing students at Goldfarb School of Nursing to caregivers who have been on the job for 20 years,” says Powers. “Stress is part of the human condition. Having the tools to deal with it is what makes the difference for living well and bringing our best to the people we serve.”